Mental Health - Clinical Guides:
Suicide Risk Assessment
How do we assess where our patient's risk is?
Assessing for Suicide Risk is something we all are doing in our practice.
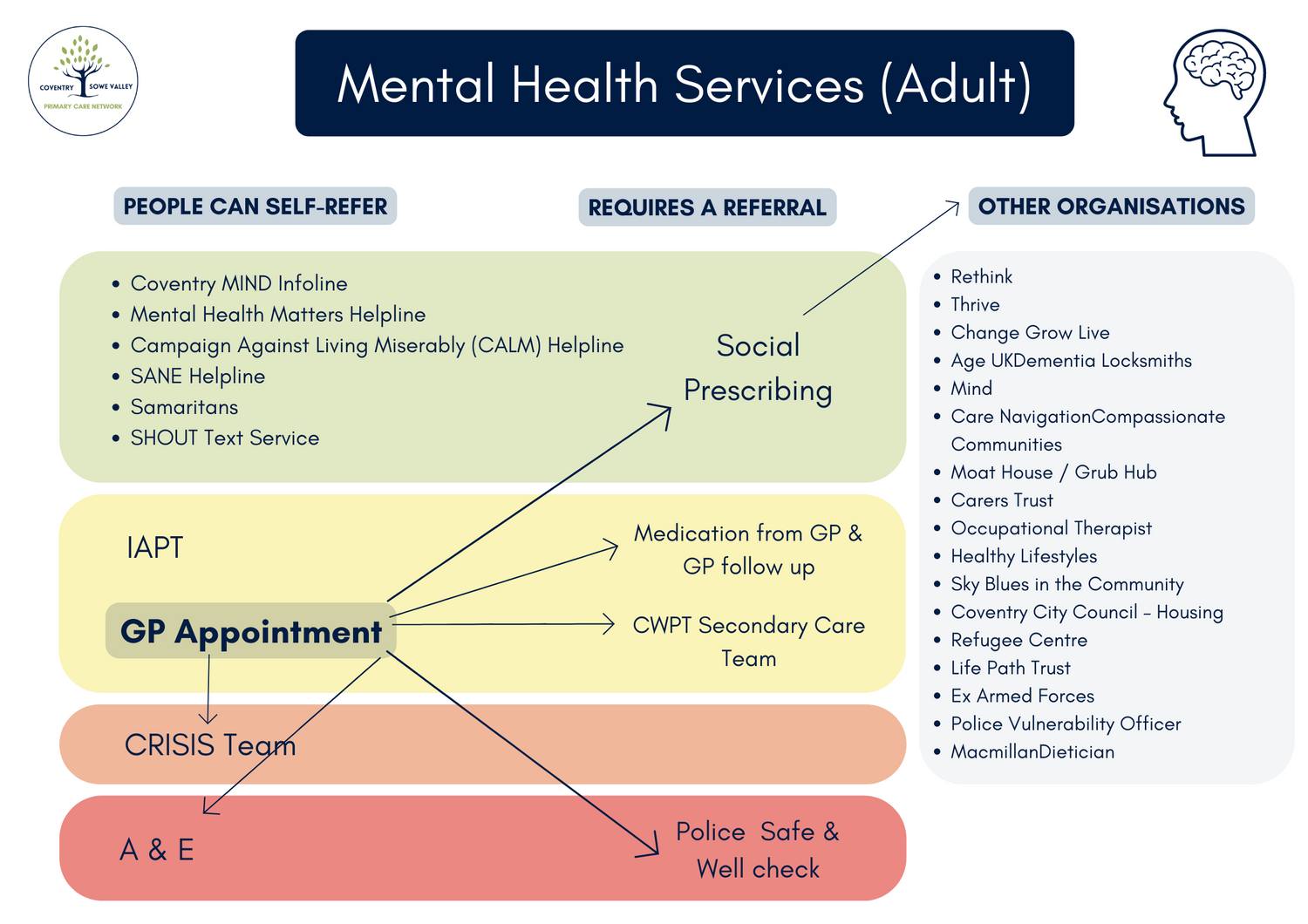
When we feel a patient is high risk - we follow guidance and refer to risk management pathways as above. But how do we decide which patients we can manage ourselves, and which patients require referral?
We know our Secondary Care Services are overwhelmed with demand, so we have to all be selective in not referring inappropriately. We also have to risk manage sensibly knowing that it may well be that the CRISIS Team for example do not get hold of the patient.
Do you feel confident that the patient will engage?

There are different approaches for assessing suicide - this is just one of them.
Having a structure in your mind about how you approach assessment can be helpful.
We have all memorised the list of questions to ask patients as per medical school but which ones do we actually use?
- Have they had thoughts that they would rather not be here?
- Are they feeling hopeless, or that life is not worth living?
– Have they made plans to end their life?
– Have they told anyone about it?
– Have they carried out any acts in anticipation of death (e.g. putting their affairs in order).
– Do they have the means for a suicidal act (do they have access to pills, insecticide, firearms…)?
– Is there any available support (family, friends, carers…)?
But one of the most important aspects is distinguishing between feelings of wanting to escape/feeling overwhelmed with a situation or wanting to actually be dead. A very difficult distinction to make.
Questions like:
- When you have thoughts of not wanting to be here, what is the nature of those thoughts?
- Do you wish you could just get away from everything eg, if someone offered you the option of just leaving abroad for a new life and never coming back would that solve your problems?
- Or do the thoughts consist more of a feeling that you would want to be dead than have to face being alive?
- Stratifying that distinction can be incredibly helpful in further questioning.
